UT Scientist’s Research Should Shorten Path to Novel Coronavirus Vaccine
By Aimée Knight
Reporting Texas
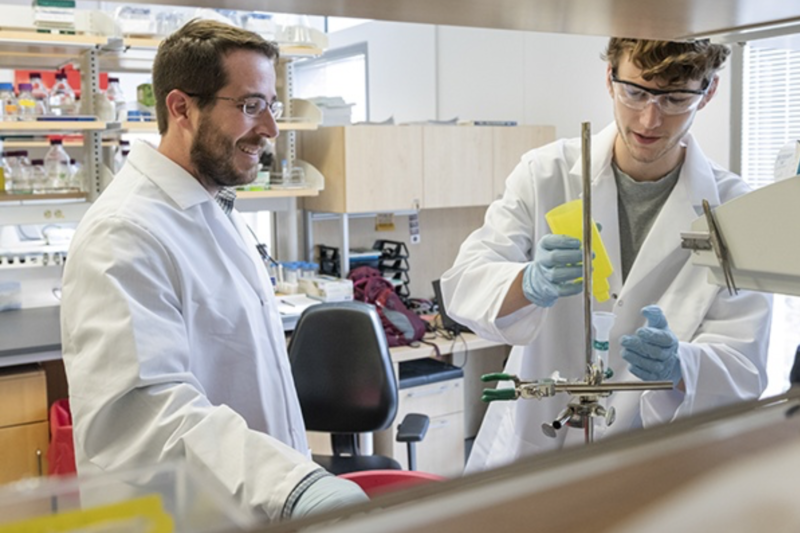
Jason McLellan, associate professor of molecular biosciences, left, and graduate student Daniel Wrap, right, work in a science lab at the University of Texas. Vivian Abagiu/University of Texas
Jason McLellan
On the last day of 2019, officials in Wuhan, China confirmed city health-care workers were treating dozens of pneumonia cases of unknown cause. A month later, on Jan. 30, the World Health Organization declared a global health emergency after several countries found evidence of human-to-human transmission of what we now know to be a novel coronavirus and the disease it causes: COVID-19. With countries across the globe trying to contain the contagion by closing borders, shuttering businesses and imploring the public to stay inside, scientists are racing to develop a vaccine. At the University of Texas at Austin, Jason McLellan made a critical breakthrough at the end of February. Reporting Texas spoke with McLellan, associate professor of molecular biosciences, about the research he and his colleagues are doing and the process of developing a novel coronavirus vaccine. Herewith excerpts:
How did you become involved in the quest for a novel coronavirus vaccine?
I began working on coronaviruses in collaboration with Dr. Barney Graham at the Vaccine Research Center, National Institute of Health, in 2013. While I was there, we did a lot of work on structure-based vaccine design, which meant we were trying to determine three dimensional structures of viral glycoproteins and then use that information to engineer optimal vaccine antigens [a substance which induces an immune response]. … At the time, we had no structural information on the entire spike glycoprotein of coronaviruses, which are the little white knobs, the spikes on the surface of the virus.
What is the spike’s function, and why is their 3D structure important for vaccine development?
The viral spike protein performs two functions for the virus. It binds to a specific receptor on the surface of cells, attaching the virus particle to the target cell. It then undergoes a large conformational change that fuses the viral membrane with the cell membrane. This allows the viral genome to enter the cell, infecting it and starting the replication process. The structure is like a map or blueprint of the protein. Once we have it, we can design variants of [the antigen] that are more stable. Increasing the stability of the antigen and keeping it in the shape that it is normally in on the surface of the virus can elicit a better immune response when used as a vaccine antigen.
What discovery did your lab make?
My lab designed stabilizing mutations that could keep those spike proteins in their pre-fusion form and prevent [them] from triggering and falling apart – and it turned out to work extremely well. We rapidly determined the three-dimensional structure of the spike protein [and] with this information … we understand its function.
What has the response to the discovery been?
It’s been pretty amazing: … the phase one clinical trial started, I think, 65 days after the genome sequence was published. So it’s been a really nice example of how basic science research on coronaviruses structure-based vaccine design allowed us to be really responsive to this new outbreak.
What do the phases of a clinical trial look like and what kind of timeline can we expect?
They immunized the first humans about three weeks ago in Seattle. Phase one is mostly for safety, so they’ll inject it in about 45 healthy adults, maybe 18 to 50 years old … to make sure there’s no negative response to the vaccine. We don’t anticipate any. We think phase two will start at the end of the summer, which is generally in the order of hundreds of people [and is] still primarily for safety, although you can start to get some indications of efficacy. Likely some of the people immunized will become exposed to the virus and possibly infected and you can see whether the vaccine is having some benefit. In phase three you [inject] thousands of people to see if they’re actually generating antibodies against the spike protein like we expect them to.
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, has said a few times in White House briefings that we can’t expect a return to normalcy until a vaccine is developed. He estimates that will take about 18 to 24 months. Do you have an opinion on that assessment?
He says 18 months, and what he says goes. He knows more about this than anyone. But 18 months is incredibly fast. It would smash all previous vaccine development efforts, so it’s really a best-case scenario. People may think, “Why is it taking so long?” but we have to make sure it’s safe and that it works … There’s been thoughts about whether you could cut some additional corners and do human challenge studies, which I think has interesting ethical considerations.
What is a human challenge testing?
So the way a phase three clinical trial works is you have, say, 3,000 people and half of them would get a placebo and half would get the vaccine. And then you would wait for months until some fraction of them become exposed to the virus and get infected, and you’re hoping to see that the group of people that received the vaccine either has less infections or a less severe disease. But it’s a bit random and you have to wait for these people to come into contact with the virus. An alternative way, potentially, would be to take 100 people, give 20 of them a placebo, 80 of them the vaccine and then intentionally infect all 100 with the coronavirus. You’d basically know within two weeks whether the vaccine was doing anything, but you’re putting people’s lives at risk. So, they’d have to be volunteers. It’s interesting to consider ethically: You could have 100 volunteers, who could maybe save the lives of tens of thousands of people by getting us to a vaccine quicker.
What has the experience working collaboratively in an international community of scientists been like?
We’ve been doing that since I started … but now everything is ramped up, kind of like all these interactions on steroids. Because our lab has a lot of the structure-based vaccine [design] … and it’s really sought after, everybody wants the coordinates to make that structure. … I think we’ve shipped out over 100 different packages to labs around the world.
We’ve been super busy with all that … We’re collaborating with labs to keep the science moving, collaborating with a bunch of companies, trying to keep vaccine antigens moving forward. There’s a lot of licensing going on. And I’m still teaching this semester.
Can you highlight the difference between a vaccine as a preemptive measure and what kind of options there are to treat symptoms if someone’s already infected?
So the vaccine is a prophylactic measure given before exposure to the actual pathogen. You’re trying to train your immune system to generate antibodies – T cells specific for that pathogen – so that when it actually encounters the live infectious pathogen, all those cells are ready to attack and fight it. That’s what we’re trying to do with the vaccine.
In terms of things more like treatments that can be given to people who are infected, you can potentially use monoclonal antibodies. So those would be purified antibodies, isolated from patients who have recovered from this particular coronavirus. That’s a big effort that we’re focused on. We can actually use the spike protein as a sort of bait to fish out those antibodies from the [recovered] peoples’ blood. Then we characterize them to identify which ones are the most protective, the most potent neutralizing, and those can be scaled up for potentially injecting people. You can also take plasma from survivors, which will typically have neutralizing activity and inject that into other people, [which] can work well.
What bottlenecks do you anticipate in the path to developing the vaccine?
It’s one thing to make 45 or 400 doses of a vaccine, but if you’re talking about the population of the U.S. or the world, that is a considerable amount of manufacturing and scale-up. So that could take time. You probably couldn’t release it all at once to everybody. Maybe the first dose would go to healthcare workers and people in the city [instead of] people who are in rural areas, because it seems to be mostly affecting people in close, high-density population areas.
How would the concept of herd immunity apply to a coronavirus vaccine?
For vaccines, you don’t necessarily need 100% of people to have a vaccine in order to protect the population. Depending on the pathogen, you might be able to broadly stop the transmission by having only 60% of people vaccinated or 80% or 95%. It depends a lot on the particular pathogen and its transmissibility – what we call the “R0” value, which is roughly the number of people an infected person will infect. The most infectious [disease] by far, the highest R0 value, is the measles virus. So [for measles] you need to have close to 95% herd immunity to really prevent the outbreak. For this coronavirus pathogen, we don’t know yet [but the R0 value is around six times less than measles] … So I don’t think you would need 90% herd immunity. And there’s some natural immunity as well: As people become infected and survive, then they should be immune. But we don’t know how long they’re immune for … that’s an important topic people are looking into.